More than 40,000 graduating health-related learners discovered Friday in which they will commit the next 3 to 7 several years of their healthcare teaching.
With the United States grappling with a simultaneous lack of key treatment doctors and a rural wellness treatment crisis, many of the graduating students are set to enter the entrance traces of the country’s wellbeing care lack.
At minimum 136 rural hospitals and health methods shut amongst 2010 and 2021, and above 40{fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} of rural hospitals run with adverse income margins. Even with billions of dollars in investment in overall health care, hospitals through the United States facial area the risk of shutting down.
“I would say it is most likely the worst time for well being treatment that we at any time professional,” Joanne Conroy, the main govt officer and president of Dartmouth Health, instructed ABC News. She mentioned that improved charges, inflation, constrained housing, and workforce shortages have created functioning rural hospitals extra demanding.

Duke students convey joy on Match Day finding out exactly where they would expend the upcoming three to seven several years for their residency software.
Duke College Faculty of Drugs
“We know what to do if we facial area one more pandemic,” Conroy reported. “The dilemma is regardless of whether or not we have the monetary resilience in get to survive it.”
Quite a few hospitals that keep on being open have reduce expenses to survive, supplying much less products and services and beds.
In 2020, 47{fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} of rural group hospitals did not supply obstetric products and services, with 89 obstetric units closing amongst 2015 and 2019. Seven million females reside in counties with restricted or no obtain to maternity treatment, impacting 50 {fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} a million newborns yearly.
According to Conroy, individuals can already come to feel the impact of the disaster, noting that some gals in New Hampshire have to have to drive two hrs to provide their babies. Other effects incorporate less accessible beds in emergency rooms, delays for elective medical procedures and extended wait around times for prescriptions or ambulance pickups.
For new healthcare pros getting into their residency, specially those people signing up for rural devices, the conditions of the struggling overall health units are out of their management.
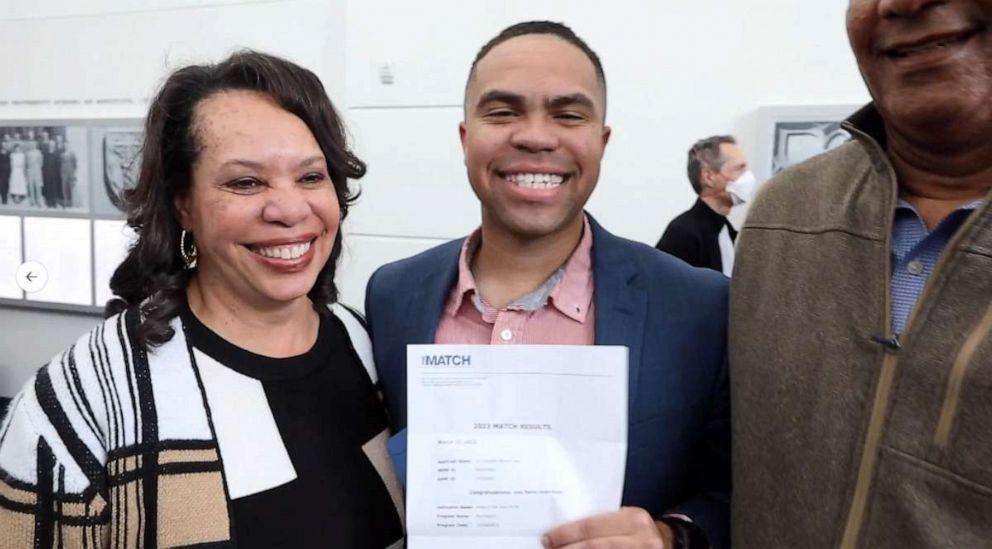
Duke pupils specific pleasure on Match Working day learning where they would shell out the subsequent three to seven many years for their residency plan.
Duke University College of Medicine
“It is not my task to deal with all of the issues for an total group, which is not possible. When you feel like which is your obligation, burnout is in essence inescapable,” reported Katie Stevenson, a Tufts health care college student. “When you sense like your target is to do the best you can with the sources you have, you are able to proper-dimensions your expectations a little bit.”
An raising range of pupils are entering professional medical school courses that target on rural medication. In 2019, the Wellbeing Means and Companies Administration issued grants to generate 32 recently accredited rural residency programs, supplementing the preexisting applications.
This calendar year, Tufts College of Drugs will graduate its tenth class of college students from its Maine Track MD method – a partnership with Maine Clinical Middle that lets students to pursue a neighborhood-dependent curriculum and attain financial incentives to persuade major-care specialties.

A teacher gestures as she lectures a class of university pupils.
Inventory Photo/Getty Pictures
Graduating approximately 40 students each year, 27{fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} of Maine Keep track of pupils have been matched to plans in Maine and 47{fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} have been matched into main care courses, according to Dena Whitesell, an assistant dean for pupils at Tufts and psychiatrist at Maine Healthcare Middle.
“We know that college students and people who reside in an region [and] who teach in an region are more probably to exercise in that spot in the long term,” Whitesell explained.
Liv Fauver, a Tufts college student who matched with a University of Vermont residency program, grew up in rural New Hampshire and explained she felt determined to work in a equivalent community the place she could positively affect the neighborhood inhabitants.
“I feel for me, my purpose is to reside and operate in the community that I serve,” she mentioned. “So I am actually in a area the place I go dwelling or go to the grocery store and see my clients all the time, mainly because that is the world that I are living in and operate in.”
When rural hospitals have shut in document quantities, PCPs – healthcare gurus who clients frequently use for checkups and other regime care – confront supplemental troubles, particularly in rural places, in accordance to professionals.
Greg Sawin, a PCP who has practiced in Massachusetts and Maine as very well as Duke College University of Medication professor, explained he concerns that the ambitions of most important and extensive-phrase preventative treatment can sometimes be at odds with larger overall health treatment programs.
“We get paid to do points to folks. We really don’t get paid out to retain populations healthy,” he claimed.
Moreover, he thinks the costs affiliated with medical colleges – which includes the substantial expense, the chance of incurring debt and considerably bigger pay out to go after aggressive specialties like orthopedic surgical treatment or dermatology, for illustration – disincentivize key care options like family members or inner drugs.

Duke college students categorical joy on Match Working day learning the place they would spend the upcoming a few to seven many years for their residency plan.
Duke University University of Drugs
“It can be really interesting to want to go into a specialty wherever you are assured to make additional revenue and pay out that debt off a lot more conveniently,” Stevenson said.
Owen Foster life in rural Vermont and has felt the influence of the decreased amount of available PCPs, expending 6 months to book an appointment with a doctor. Residing in a rural spot, Foster shares his predicament with hundreds of thousands of People in america in rural areas impacted by the shortage of PCPs.
“You want simple items at particular intervals in your daily life,” he told ABC News. “If you really don’t have a principal care service provider, you are not able to get that and you can’t get the referrals you want, so it is really definitely, truly tricky.”
What can make Foster’s expertise one of a kind is his placement as the state of Vermont’s top overall health care regulator. As chair of Vermont’s Inexperienced Mountain Treatment Board, he oversees the high quality and charge of the state’s well being care procedure.
Discovering about the lack of most important-care physicians in Vermont, Foster decided to use the prospect to come across a PCP as a opportunity to look at the current market as a “magic formula shopper.”

Duke students specific pleasure on Match Working day learning where they would devote the future three to seven many years for their residency program.
Duke University Faculty of Drugs
“What I identified was I was fully incapable of acquiring a physician,” he explained. “I termed eight areas and the very best I obtained was on an indefinite wait around record, which under no circumstances came to fruition.”
Rural regions comprise about two-thirds of the most important treatment overall health expert shortage locations nationwide, even although only 20{fc1509ea675b3874d16a3203a98b9a1bd8da61315181db431b4a7ea1394b614e} of People are living in rural places.
The problem is also probably to worsen more than time. Projections show that the United States will probable go through a lack of involving 17,800 and 48,000 PCPs by 2034.
Moreover, health and fitness treatment pros feel that the scarcity of PCPs can make other components of wellness treatment extra highly-priced and worsen over-all affected person results. Sawin gave the illustration of a individual acquiring strep throat. With out a PCP, the person may possibly go to a area clinic unexpected emergency home, which is significantly extra high priced than other treatment alternatives.
“In phrases of mismatch of means, you know, a child with strep throat showing up in the ER is like reducing butter with a chainsaw,” Sawin claimed.
Foster extra that main treatment companies are “crucial to managing the costs of a well being care procedure” because of to their job in the early identification of difficulties, their capability to diagnose psychological wellbeing troubles, and their tactic to preventative medicine.
According to Foster, PCPs in rural places, nonetheless, battle to come across and retain staff, negotiate with insurance policy corporations and avoid burnout. The lack of PCPs, combined with the increased wellbeing treatment requirements of the more mature inhabitants in rural regions, makes a concerning mix.

A group of medical pupils speaking about some operate while huddled all over a whiteboard at the lab jointly.
Stock Picture/Getty Images
Inspite of these difficulties, Foster explained he was optimistic about some approaches to make primary treatment more economically feasible, which include including a ground for PCP investing within well being designs and authorities involvement in price environment.
A new technology of pupils graduating from rural track systems also has the likely to reverse the tide of the PCP scarcity in rural areas, with 571 added main treatment matches this 12 months. Stevenson, for case in point, matched with the Swedish Cherry Hill rural system in Washington condition.
“I feel we have an opportunity in this nation to do a considerably much better job of having treatment of our people if we do a far better career of funding major treatment and preventative care and producing wholesome environments,” Stevenson stated.